Fact or Fiction: 6 Myths About COVID-19
As scientists continue to learn more about COVID-19, the world faces a double threat: the spread of the virus, and the spread of misinformation around it. Here are some common myths related to the virus.
Though COVID-19 has been with us for more than two years now, researchers are still working to understand and treat the virus, with major questions about its transmissibility, immunity, and impact still being studied.
We know much more about the disease than we did at the beginning, and with vaccines now widely available — and hundreds of additional coronavirus vaccines in development — our knowledge about the virus is growing rapidly. Still, as the virus continues to threaten millions of lives across the globe, so does a host of myths about the disease: a “pandemic of misinformation” distracting from reliable public health guidance.
As with any disease, the more we know the more we are able to prevent and contain its spread. So what’s fact, what’s fiction, and what’s to be determined? Here are six common misconceptions about COVID-19.
Myth #1: The vaccine isn’t safe.
Fact: The COVID-19 vaccines followed the same process all vaccines do and showed no major safety concerns in trials.
The spread of COVID-19 demanded an unprecedented vaccine pipeline, and researchers have responded: less than one year after the first recorded case in the U.S., the CDC authorized two vaccines for use. One was developed by Pfizer, and the other by Moderna. Three other vaccines are in Stage 3 clinical trials.
All vaccines go through rigorous safety testing, including these fast-track vaccines that were developed quickly. The FDA sets rigorous safety standards for vaccines to meet before they are approved, which include four phases. This infographic from the FDA explains the four stages and how many volunteers received the virus at each stage before it could advance. Even though these vaccines were developed fast, they didn’t skip any steps in that process.
Neither the Pfizer nor Moderna vaccines showed any major safety concerns in their trials, and each one was monitored by an independent safety board. They do not carry the live virus, meaning you can’t catch COVID-19 from the vaccine. Most importantly, each vaccine showed about 95% efficacy at preventing mild and serious symptoms of COVID-19.

Myth #2: You don’t need the vaccine if you’ve already had the virus.
Fact: Natural immunity doesn’t last forever, and you can catch COVID-19 again.
For those who recover from COVID-19, research shows that immunity can begin to wane as little as three months after infection. The transmissibility of variants like omicron makes reinfection more likely than it did at the beginning of the pandemic.
As researchers continue to study COVID-19 variants, the best ways to protect yourself are to get vaccinated and boosted as soon as you are eligible.
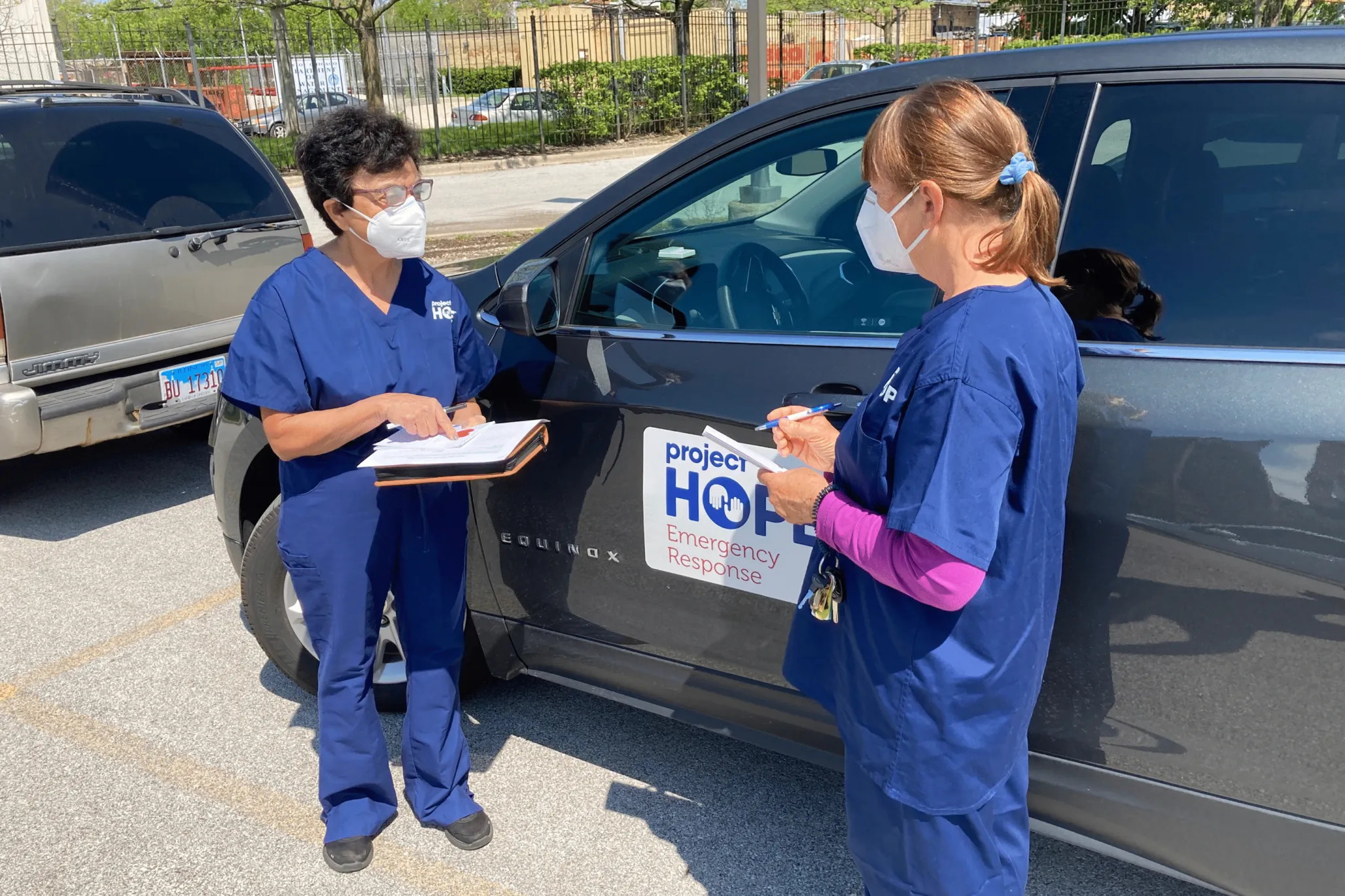
Myth #3: Masks don’t work.
Fact: Wearing a mask remains one of the most basic ways to prevent the spread of the virus.
There is clear evidence that masks help prevent the spread of COVID-19, including a 2020 study from our Health Affairs journal which found that state mask mandates led to a slowdown in the daily COVID-19 growth rate.
Anyone over the age of 2 should wear a mask covering the mouth and nose when out in public — and maintain physical distance of at least six feet from others.
Myth #4: Kids can’t spread the virus.
Fact: Children can both catch and spread the virus.
A study out of Harvard found that infants, children, and adolescents are just as likely as adults to carry high levels of the virus. Though most children who catch COVID-19 are more likely to be asymptomatic, they are still carrying the live virus and can spread it to others. Because variants like omicron are more transmissible, that means the best way to prevent the spread of the virus continues to be masking and other public health measures.

Myth #5: We can achieve herd immunity by letting the virus spread in the community.
Fact: Herd immunity through natural infection is unlikely. Vaccines are the best way to eliminate it.
Herd immunity occurs when enough people in a community contract and recover from a virus that they develop the natural immunity to protect them from the disease going forward. In order for it to be effective, about 70% of people have to contract and recover from the disease. But there are major reasons why this will not work with COVID-19.
First, we don’t know how long immunity lasts, though recent research shows it could be as little as three months thanks to variants of the virus.
Second, while vaccines against COVID-19 are very effective at preventing serious illness, they do not totally prevent you from catching the virus. As these professors from Johns Hopkins put it: People who have gotten vaccinated can still become infected, and some people who have had COVID-19 can get it again. With vaccine numbers lagging nationwide, that makes it harder to reach levels of herd immunity that would wipe out the virus for good.

Myth #6: We know COVID-19 doesn’t cause long-term damage.
Fact: It can be a long road to recovery, and scientists are just beginning to research the lingering effects.
Fatigue, shortness of breath, persistent loss of sense of smell, and damage to the heart, lungs, kidneys, and brain are just a few symptoms on a long and wide-ranging list of the lingering effects of COVID-19.
Researchers are still working to understand “long COVID,” or post-COVID-19 syndrome. For now, three types of long COVID have emerged: people who do not recover completely, people who have to recover from long periods of hospitalization, and people who experience symptoms after recovery. In addition to symptoms like loss of taste or smell, many people also experience brain fog, anxiety, depression, shortness of breath, or even skin conditions.
As researchers continue to study COVID-19 and its long-term implications on our health, the most important tools to prevent it are getting vaccinated and following all public health guidance.



